Ankylosing spondylitis – Basics for patient
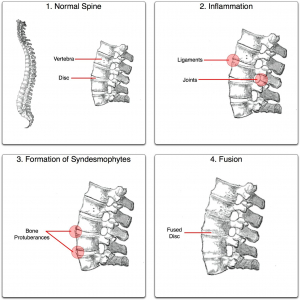
Ankylosing means – Fusion.
Spondylitis means – Inflammation around spinal vertebra or in spine joints
Ankylosing spondylitis is a disease that usually starts with pain and inflammation in lower back region. It is a type of arthritis.
Generally, it is believed that arthritis is a disease of old age. Rheumatology is a medical field that involves many types of arthritis. Rheumatologist is a doctor who detects these types of arthritic diseases and treats them. There are a lot of rheumatic diseases that one can develop at very young age. AS is such a disease.
Ankylosing spondylitis begins with swelling in the sacro-iliac joint, which is a part of spine joint (Picture 1). There are two sacro-iliac joints in the body near each buttock region. This inflammation of sacro-iliac joint is known as sacro-ileitis. However, As patient can have inflammation of many other areas in spine to start with or later in the disease. Other joints of the body like knee, ankle etc may also be involved. It usually affects young males and females and disease usually starts before 45 years of age. It can also affect children and teenagers (< 16 years ) of age in a slightly different form. Males are more commonly affected than females. Occasionally, this disease can lead to fusion of spine vertebra (Picture 2).
Ankylosing spondylitis is a type of arthritis, which usually affects adolescents or young people and starts with back pain or hip pain. It is usually associated with pain and stiffness on prolonged rest, sleeping and while getting up in morning.
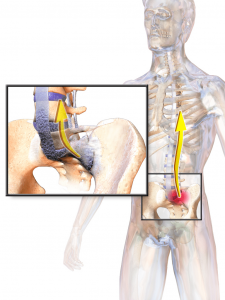
The most common symptom of this is lower back pain (Figure 1).
This lower back pain usually
- Starts before the age of 45
- Builds up slowly over weeks
- Lasts longer than 3 months
- After resting, the pain and stiffness increases – like when lying/sleeping at night and while getting up in the morning
- Pain and stiffness usually decreases with some activity or exercises
The commonest symptom of ankylosing spondylitis pain and stiffness in lower back or buttock region, which increases on rest (especially when lying down at night and getting up in morning) and decreases with activity (walking or exercise). Often, in early phases, a patient of Ankylosing spondylitis, can play sports or do exercises without problems, but can’t sleep in night due to back pain.
Other symptoms
- Excess fatigue whole day
- Pain, swelling and stiffness in other joints of the body – like hips, knee, ankle, shoulders, foot etc
- Pain and swelling in other parts of body like heel (plantar fascitis), achilles tendon (back of the heel), side of the hips, pain in ribs / chest pain during breathing etc
This disease can be sometimes associated with some other problems/diseases like
- Iritis / Uveitis – About 30 % of AS patients can have attacks of pain, swelling and redness in one or both eyes. This is often associated with blurred vision and clears with steroid drops. These attacks can be recurrent.
- Inflammatory bowel disease – 5-20 % of AS patients have an associated bowel problem which is associated with pain in abdomen, bleeding in stools and diarrhoea. This bowel problems may start even before ankylosing spondylitis starts. There are two such disease, Ulcerative colitis and Crohn’s disease. These diseases are associated with inflammation or swelling in bowel, hence known as inflammatory bowel disease.
There is no single test that can tell you have AS with 100 percent guarantee. A Rheumatologist diagnoses Ankylosing spondylitis by getting a complete picture from your history and a combination of various tests.Read more : What is HLA b27 ? What does it mean ? Is it curable ?
- Pain and stiffness are quite severe and increasing in intensity, they are affecting daily functioning.
- Hip pain – Any ankylosing spondylitis patient with hip pain is likely to have severe disease
- Increases ESR and CRP in blood reports is usually a sign that your disease is active
- MRI continues to show inflammation or swelling even after preliminary treatment
Many people may need to take one or more medicines for Ankylosing spondylitis:
NSAIDS (Non-steroidal, anti-inflammatory drugs) – This is a large group of medicines which include Ibuprofen (Sample Brand Name: Brufen) and Naproxen (Sample Brand Name: Naprosyn), Indomethacin (Sample Brand Name: Donica, Inmecin), Etoricoxib (Nucoxia, Arcoxia), Celecoxib etc. These medicines can help in relieving pain. Though, called pain killers by general population, they are actually anti-inflammatories. Basically they help reducing pain, swelling and inflammation in patients with Ankylosing spondylitis patients. If given in the correct amount and in the right way, then they can be very beneficial. Other medicines – There are other medicines (Sulfaslazine – Saaz, Methotrexate – Folitrax), Biological injections – Infliximab (Sample Brand Name: Remicade) ; Adalimumab (Sample Brand Name: Humira, Exemptia); Etanercept (Sample Brand Name: Enbrel, Intacept, Etacept), Secukinumab (Cosentyx, Scapho) which can help in treatment of symptoms and prevent complications. Your doctor or nurse will decide which medicines are best for you. Read more : Is it safe to have biologics for Ankylosing spondylitis ?- Stop Smoking – If you smoke and you have AS, it is more likely to make your disease worse and more likely to cause respiratory problems. Quitting smoking can help you control the disease.
- Eat healthy. There is no need for any diet or stop anything in patients with ankylosing spondylitis.
- Exercise – Physiotherapy / Exercise – Follow your physiotherapist’s doctor’s instructions for exercise and stretching. Stretch regularly at work.
- Get Calcium and Vitamin D in the right amount – it can help to protect your bones from being weak. Your rheumatologist will help you with knowing what is the right intake for you.
- Get as much information as you can, exact knowledge about the disease will help you to avoid wandering from the right treatment. Don’t fall into traps of people claiming to cure your AS, in some patients AS goes silent on its own. That doesn’t mean somebody has cured it.
- Continue regular follow ups with your Rheumatologist who is an arthritis specialist.
How will ankylosing spondylitis affect my future life ?
As Ankylosing spondylitis often starts in teenagers or young adults, its affects their study and high earning years. The chronic pain can be frustrating for many in these important years. The good news is that, in today’s era, with very good treatment, most people with AS can have a reasonably good life .
30-50% of AS patients generally do not have very serious or severe symptoms. They can mange life with intermittent ant-inflammatories and exercises alone. Also, some times you might have a different arthritis called reactive arthritis and might be labelled as ankylosing spondylitis. This is actually quite a common occurrence in a developing country like India, where most people with arthritis don’t see rheumatologist (Read below on why the two are often confused with each other). The good thing about reactive arthritis is that it usually subsides in three months.
In many patients disease can have periods of activity and inactivity. When their disease flares / becomes active they have pain and might have to take necessary medications. In many such patients with intermittent complaints, disease often goes into silence between this flare episodes.
In 30-70% of the population the disease can be very active. Such patients have difficulty managing their lives smoothly. If such patients don’t take proper treatment they might have fusion of spine or damage to hips. So always try to follow your treating rheumatologist’s advice.
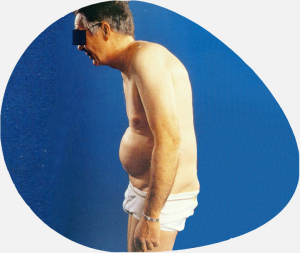
- AS patients with very active disease can have fusion in spine vertebra with forward stopping posture in future.
- Active AS patients not taking proper treatment can have hips or other joints damaged, which can give chronic pain and walking difficulties. Such patients might need hip replacements at a young age.
- Some AS patients can have recurrent inflammatory attacks in eye, known as iritis or uveitis. If not treated properly it may cause complications in eye.
- In AS patients, who have had spine fusion and very active disease, their spines can be very stiff from outside and weak from inside (thin internal bone structure). This can make them very prone to spine fractures even with minor falls. They should always consult respective doctors, if they have had a fall and continuous pain.
- Very rarely, chronic AS patients can develop loosening one of the heart valves causing it to leak. This usually happens in AS patients who have had disease for more than 20-40 years.

Most of above AS complications are avoidable or treatable, provided they take proper treatment. So please have regular follow-up with your treating doctor.
Yes, it is certainly possible. Both male and female AS patients can conceive normally and there is no increased risk of anything to the baby. In the modern era, most young AS patients can have normal pregnancies with healthy babies. However, one has to tell their doctor if they are planning a pregnancy. Certain drugs need change / planning before pregnancy planning begins. Do not wait till you or your partner gets pregnant, tell your rheumatologist even when you are thinking of same. They will guide and adjust medications. For females, it is better to plan pregnancy when your disease is controlled and your rheumatologist is happy for you to plan the same.
References
- https://www.prnewswire.com/news-releases/abbvies-humira-adalimumab-receives-us-food-and-drug-administration-approval-to-treat-adults-with-non-infectious-intermediate-posterior-and-panuveitis-300293114.html
- HUMIRA Injection [package insert]. North Chicago, IL: AbbVie Inc.
- HUMIRA [Summary of Product Characteristics]. AbbVie Ltd. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000481/human_med_000822.jsp&murl=menus/medicines/medicines.jsp&mid=WC0b01ac058001d124. Last updated June 16, 2016. Accessed April 21, 2018

